Digital Pathology’s Impact on Personalized Cancer Therapy
Cancer treatment is a complex process. It involves medical interventions and therapies to control, cure, or manage the disease. Cancer is a disease characterized by the uncontrolled growth and spread of cells in the body. With advances in scientific research, technology, and medical knowledge over time, considerable progress has been seen in treating cancer.
The Evolution of Cancer Treatment
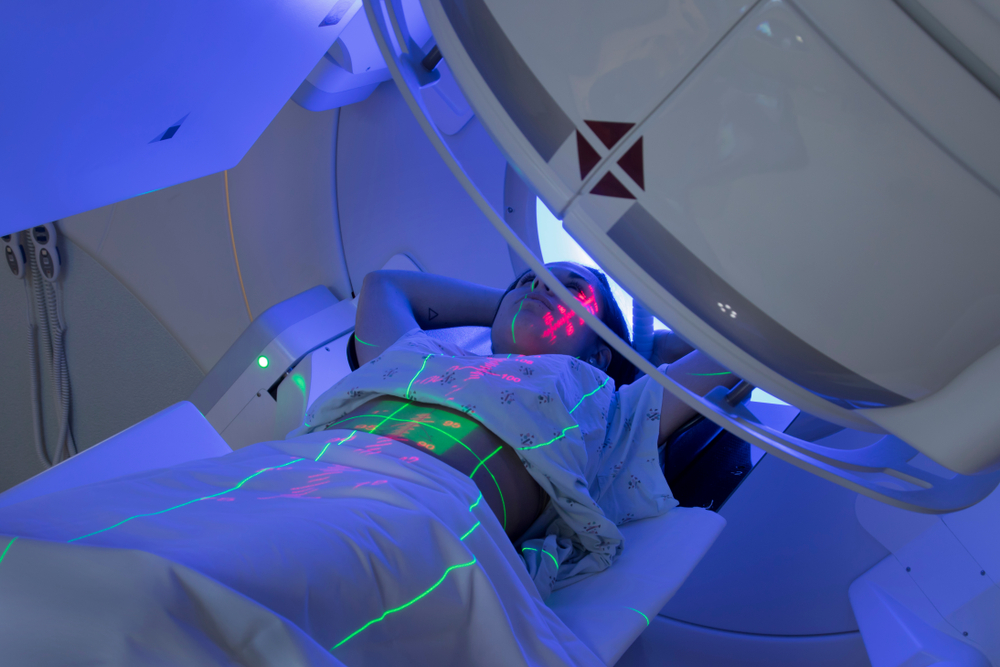
Historically, surgery was the main treatment for cancer. To treat the disease, surgeons used to remove the tumor and surrounding tissue. A major advance in the early 20th century was radiotherapy, which uses high-energy radiation to target and destroy cancer cells. Later, chemotherapy became the cornerstone of cancer treatment. This treatment option uses drugs to kill or stop the growth of cancer cells throughout the body.
In recent decades, the understanding of cancer biology and genetics has expanded, leading to the development of targeted therapies. These treatments target molecular abnormalities or genetic mutations in cancer cells to inhibit their growth or promote their destruction while sparing healthy cells. Targeted therapies have shown significant success in certain types of cancer with improved outcomes and reduced side effects compared to conventional treatments.
Immunotherapy has emerged as another pioneering approach. It uses the body’s immune system to recognize and attack cancer cells. Immunotherapy has shown remarkable efficacy in various malignancies and has changed the treatment landscape for certain types of cancer. Moreover, advances in precision medicine and genomic profiling have enabled personalized cancer treatment. By analyzing a tumor’s genetic makeup, doctors can identify specific mutations or biomarkers and alter treatment accordingly. This approach helps optimize treatment outcomes and minimize side effects.
In addition, innovative techniques such as minimally invasive surgery, robotic surgery, and image-guided radiation therapy have increased treatment accuracy, reduced complications, and improved patient recovery.
Over the years, cancer treatment has evolved from primarily relying on surgery, radiotherapy, and chemotherapy to a more comprehensive and targeted approach. This advancement in the field of cancer treatment has the potential to improve patient outcomes in the fight against cancer. In this blog, we will explore everything about personalized cancer therapy approach, the impact of digital pathology on personalized cancer treatment, and digital pathology solutions for cancer diagnosis.
What Is Digital Pathology and How It Works?
In today’s time, digital pathology has shown a significant impact on personalized cancer treatment, revolutionizing the way pathologists analyze and interpret cancer specimens.
What is digital pathology?
The digital pathology process introduces a new paradigm in pathology by leveraging automation, digital imaging, and AI technologies. It addresses the limitations of the standard process, such as error rates, manual handling, and the potential for diagnostic inaccuracies, by providing a streamlined, efficient, and data-rich environment.
The Role of Digital Pathology in Personalized Cancer Treatment
Digital pathology solutions for cancer diagnosis provide significant advancements in accuracy, efficiency, and collaboration.
- High-Resolution Imaging: Digital pathology systems capture high-resolution images of tissue specimens, providing clinicians with an unprecedented level of detail that is not easily seen through traditional microscopy.
- Image Analysis Tools: Digital pathology platforms provide pathologists with image analysis tools and algorithms to aid in the detection and quantification of specific characteristics or anomalies within tissue samples.
- Second Opinions and Collaboration: Digital pathology facilitates the easy sharing of digital images for second opinions and consultations among pathologists, regardless of their physical location.
- Comparison and Follow-up: Digital pathology allows pathologists to compare current digital images with previous cases and follow-up samples from the same patient. The ability to compare digital images side-by-side improves diagnostic accuracy and improves patient management.
- Integration with Molecular Data: Digital pathology can be integrated with molecular data such as genetic profiles and immunohistochemistry results. It provides a complete overview of the tumor’s molecular characteristics and is useful for subtyping, determining prognosis, and identifying potential targeted therapies.
- Educational Resources and Quality Assurance: Digital pathology provides extensive educational resources, including access to large collections of digital slides for training and reference purposes.
Considering all of the above points, it is fair to say that digital pathology technology helps increase diagnostic accuracy, reduce subjectivity, and promote standardized practice, ultimately leading to improved patient outcomes. It provides valuable insight into the molecular characterization of diseases and guides targeted therapies, making a significant contribution to the advancement of personalized medicine.
Advantages of Digital Pathology
Digital pathology for cancer treatment offers several benefits over traditional pathology methods. Here are some key advantages:
- Enhanced accuracy and precision: Digital pathology systems capture high-resolution images of tissue samples, providing pathologists with detailed, zoomable views. This improves accuracy in identifying cell structures, architectural patterns, and subtle abnormalities.
- Efficient remote collaboration: Digital pathology enables pathologists to share cases and collaborate remotely. With digital images accessible from anywhere, experts can more conveniently conduct consultations, provide second opinions, and participate in multidisciplinary oncology committees.
- Integration with data analytics and artificial intelligence (AI): Digital pathological images can be analyzed using AI algorithms and data analysis techniques. This enables automated image processing, pattern recognition, and identification of biomarkers and genetic variants.
- Efficient archiving and retrieval of patient data: Digital Pathology eliminates the requirement to physically store and retrieve slides. Digital images can be stored securely in a centralized database, ensuring long-term access and easy retrieval for future reference, research, or retrospective analysis.
- Facilitation of telepathology and teleconsultation: Digital pathology allows remote diagnosis and consultation, especially in areas where access to pathology expertise is limited. Telepathology lets specialists remotely review digital images, provide quick diagnoses, and make treatment decisions.
- Support for research and education: Digital pathology facilitates the sharing of anonymized datasets for research purposes, enabling significant studies, biomarker discovery, and predictive modeling. It also provides valuable educational resources, giving trainees and students access to a wide range of digital slides to advance their pathology learning and proficiency.
- Improved communication with patients: By leveraging the technology, healthcare providers can improve communication with patients by utilizing visual representations, facilitating remote consultations, providing patient access to reports, offering educational resources, enabling second opinions, and allowing real-time communication.
Overall, with all these benefits digital pathology accelerates the diagnostic process and reduces errors. Ultimately, it contributes to more accurate diagnosis, personalized therapeutic approaches, and improved patient care in the field of cancer treatment.
Challenges and Limitations of Digital Pathology
While digital pathology offers several benefits, there are also some challenges and limitations associated with its use in cancer treatment. Here are a few key challenges:
- Technical infrastructure requirements: Implementation of a digital pathology system requires significant technological infrastructure such as high-resolution scanners, storage capacity, and network connectivity. Building and maintaining such infrastructure can be costly and difficult, especially for small or resource-constrained healthcare facilities. It also needs an update of outdated IT systems and networks.
- Standardization and interoperability: The lack of standardized protocols and formats for image acquisition, storage, and analysis can impact interoperability between systems from different vendors. This may limit the ability to effectively share and integrate digital pathology data.
- Image file size and storage: Digital pathology images can be large files that require considerable storage space. Managing and storing these large files can be challenging, especially for institutions with limited storage or cloud computing infrastructure.
- Validation and regulatory considerations: Validating the accuracy, reliability, and performance of digital pathology systems is critical to ensuring clinical utility. Also, the regulatory guidelines and requirements for digital pathology are still evolving. Complying with these regulations and obtaining the necessary permits can be a complex process.
- Workflow integration and adaptation: Integrating digital pathology into existing clinical workflows requires careful planning and adaptation. Migration may require changes in laboratory practices, training programs, and quality control measures. Adapting to new technologies and workflows can initially disrupt established routines and require extra effort for a smooth adoption.
- Legal and ethical considerations: Digital Pathology involves dealing with sensitive patient data. Adherence to legal and ethical guidelines regarding data protection, patient consent, and data sharing is paramount. Protecting patient information and ensuring secure data transmission and storage are ongoing challenges in the field of digital pathology.
As digital pathology continues to evolve, addressing these challenges will pave the way for broader implementation and improved integration into cancer treatment pathways.
Future of Digital Pathology in Cancer Treatment
The future of digital pathology in cancer treatment holds great promise for advancements in diagnosis, personalized medicine, and patient care. Here are some key areas where digital pathology is expected to play a significant role:
- Artificial intelligence and machine learning: Integration of artificial intelligence (AI) and machine learning algorithms with digital pathology has the potential to revolutionize cancer diagnosis and treatment. These technologies have the potential to enhance diagnostic accuracy, optimize treatment selection, and improve patient outcomes.
- Precision medicine and targeted therapies: By enabling the identification of specific biomarkers, genetic mutations, and tumor characteristics, digital pathology facilitates the selection of precision medicine targeted therapies tailored to individual patients.
- Integration with genomic data: Integrating digital pathology with genomic data analysis will enhance the understanding of the molecular profile of tumors. This integration will further personalize treatment decisions and help guide targeted therapies based on the genetic makeup of individual tumors.
- Telepathology and remote consultations: Digital pathology will continue to expand the reach of pathology expertise through telepathology and remote consultations. This will improve access to specialized pathology services and enable timely and accurate diagnoses.
- Big data analytics and research: Digital pathology generates vast amounts of image and patient data, which can be leveraged for big data analytics and research.
- Digital pathology in clinical trials: Digital pathology will play a crucial role in clinical trials by providing standardized and objective assessments of tissue specimens. This will accelerate the development of new therapies and help bring innovative treatments to patients faster.
Overall, the future of digital pathology in cancer treatment holds immense potential for enhancing diagnosis, treatment selection, and patient care.
To summarize,
Digital pathology solutions for cancer diagnosis have the potential to revolutionize personalized cancer treatment in the form of enhanced diagnostic accuracy, improved treatment selection, real-time treatment monitoring, facilitating clinical trials, data-driven decision-making, remote consultations and collaborations, and more.